Understanding the Timeline: When Dry Socket Actually Develops
Can you get dry socket same day as extraction? Here's what you need to know right away:
Quick Answer:
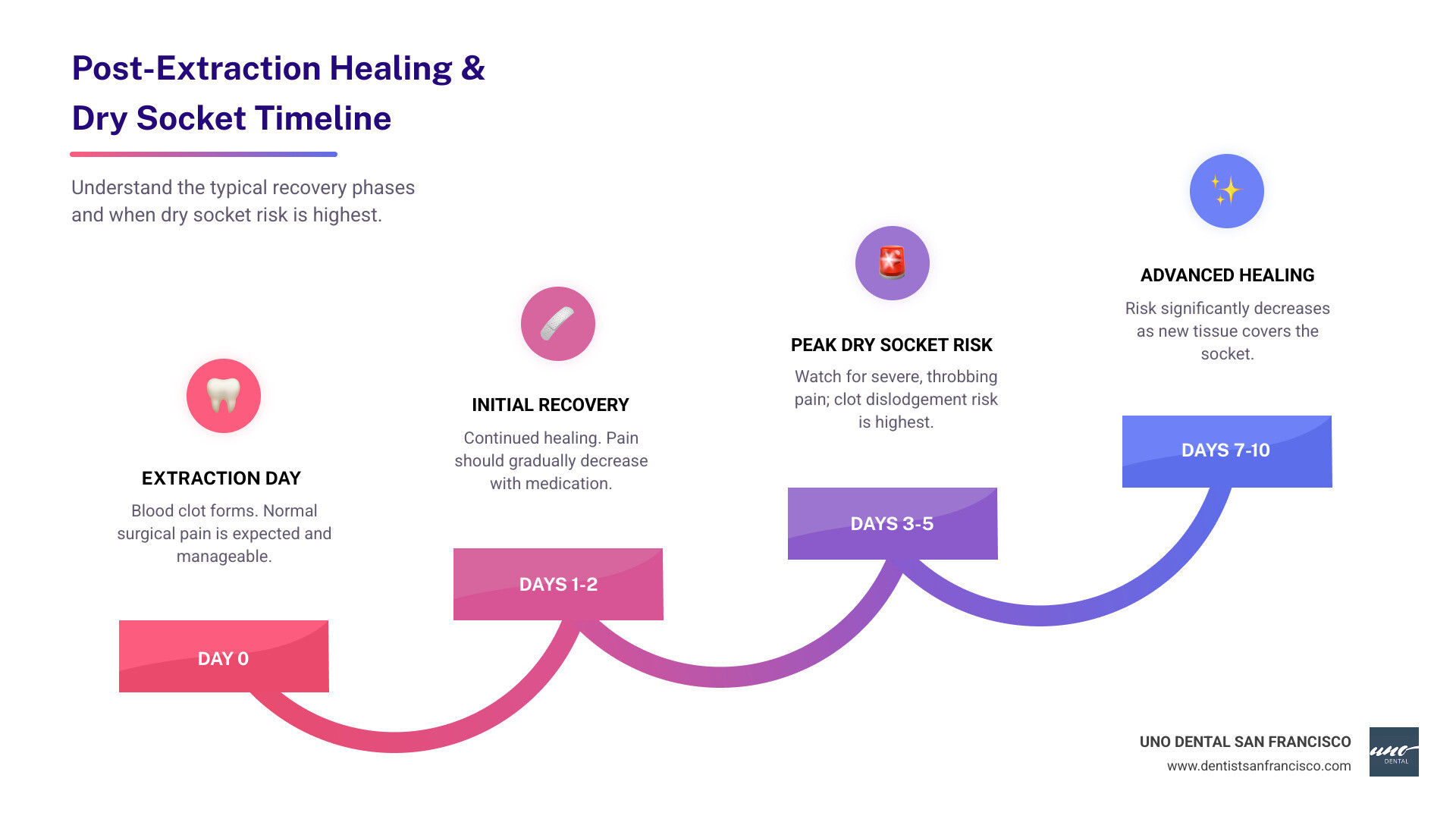
- No, dry socket on the same day is extremely unlikely
- Dry socket typically develops 1-3 days after extraction, with most cases appearing on days 3-5
- Same-day pain is normal post-surgical discomfort, not dry socket
- The blood clot needs time to form and then dislodge for dry socket to occur
If you've just had a tooth pulled, worrying about every twinge of pain is common. Many patients wonder if the discomfort they feel hours later means something went wrong. The good news is that immediate pain is completely normal. Dry socket, while uncomfortable, follows a predictable timeline that rarely starts on day one.
The research is clear: most cases of dry socket develop within roughly 3-5 days after surgery. The typical onset is on the third or fourth day after extraction, not within the first 24 hours. This is because dry socket occurs when the protective blood clot at the extraction site becomes dislodged or dissolves before the wound has healed, and this process simply takes time.
Understanding this timeline can save you unnecessary worry. While it's important to watch for warning signs, knowing what's normal versus what requires a call to your dentist helps you heal with confidence rather than anxiety.
At UNO DENTAL SAN FRANCISCO, our dentists have guided hundreds of patients through post-extraction recovery. With over 15 years of experience in restorative and surgical dentistry, we've seen that patient education about healing timelines significantly reduces anxiety and improves outcomes. Every tooth extraction at our San Francisco practice includes clear, customized aftercare instructions and the option for follow-up support, including virtual check-ins when appropriate, so you are never left guessing about what is normal.
Basic can you get dry socket same day as extraction terms:
- can i brush my teeth same day as tooth extraction
- can i eat the same day after tooth extraction
- can i get a tooth extraction the same day
What is a Dry Socket vs. Normal Healing?
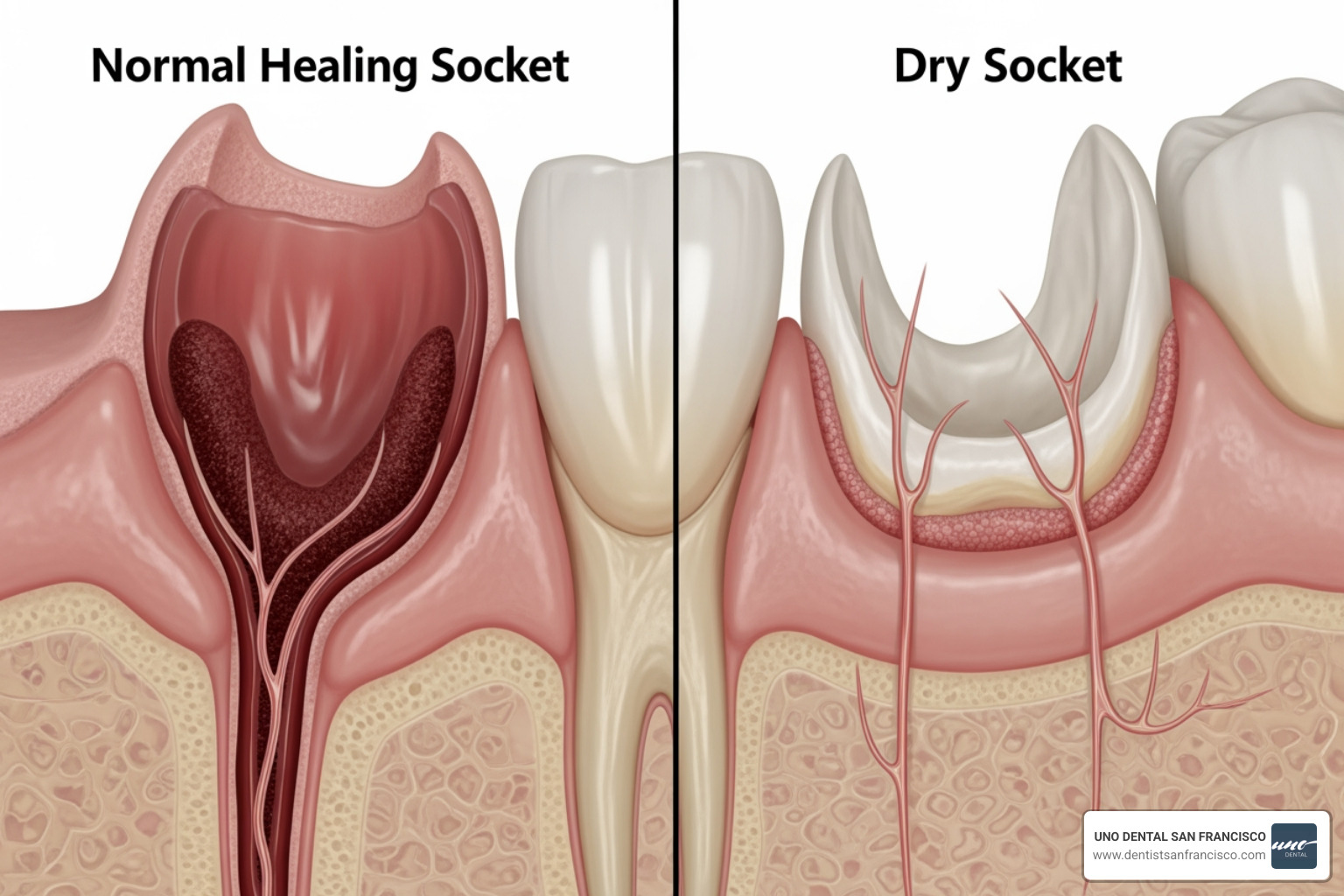
After a tooth extraction, our primary goal is a smooth, comfortable healing process. A critical part of this healing is the blood clot that forms in the empty socket. This clot is a vital protective barrier, shielding the underlying bone and nerve endings. It also serves as the foundation for new tissue growth, helping the socket close naturally.
In normal healing, the blood clot remains firmly in place, gradually replaced by healthy gum tissue and bone. The pain you experience after the extraction will steadily decrease, and you'll notice a dark red clot in the socket.
A dry socket, medically known as alveolar osteitis, occurs when this essential blood clot is lost prematurely. Without this protective barrier, the sensitive bone and nerve endings are exposed to air, food, and bacteria. This exposure leads to inflammation and significant pain, distinct from normal post-surgical discomfort.
To help you understand the difference, here's a comparison between a normally healing socket and a dry socket:
| Feature | Normal Healing Socket | Dry Socket (Alveolar Osteitis) |
|---|---|---|
| Pain Level & Timeline | Pain decreases over time, manageable with medication. | Severe, throbbing pain that often increases after 2-3 days. |
| Appearance of Socket | Dark red blood clot visible, socket may look slightly dark. | Socket appears empty, bone may be visible as a whitish area. |
| Taste & Breath | Mild or no bad taste, normal breath. | Foul taste in the mouth or bad breath. |
| Healing Progression | Socket gradually closes, gum tissue begins to cover. | Delayed healing, exposed bone remains vulnerable. |
| Radiating Pain | Localized to the extraction site. | Pain can radiate to the ear, eye, temple, or neck on the same side. |
The Critical Role of the Blood Clot
The blood clot that forms immediately after a tooth extraction is nothing short of miraculous. Think of it as the first brick in the wall of your body's repair process. It does several crucial jobs:
- Wound Protection: It acts as a physical shield, guarding the delicate exposed bone and nerve endings against irritants like food debris, saliva, and bacteria.
- Foundation for New Tissue: The clot provides a scaffold, a natural framework upon which new gum tissue and bone can grow and regenerate. Without it, the healing process is significantly hindered.
- Preventing Infection: By sealing off the wound, the clot helps prevent bacteria from entering the deeper tissues, reducing the risk of infection.
- Nerve Ending Coverage: The sensitive nerve endings in your jawbone are left exposed after an extraction. The blood clot covers these, preventing the intense pain associated with dry socket.
When this clot is lost, the underlying bone and nerves are left vulnerable. This exposure is what causes the characteristic, intense pain of a dry socket, which can be significantly more severe than the initial surgical discomfort. It's a clear sign that the body's natural healing process has been disrupted.
Normal Post-Extraction Pain vs. Dry Socket Pain
It's natural to experience some pain and discomfort after a tooth extraction. After all, it's a surgical procedure! This normal post-extraction pain usually peaks within the first 24 to 72 hours following the surgery. It's often described as a dull ache or soreness, and it should be manageable with over-the-counter pain relievers like ibuprofen or acetaminophen, or any prescription medication we might provide. Importantly, this pain should gradually improve with each passing day. Bruising, swelling, and inflammation are also common and part of the normal recovery.
However, the pain associated with a dry socket is a different beast entirely. Instead of improving, the pain typically starts to worsen, often becoming severe and throbbing, usually 1 to 3 days after the tooth is pulled. This intense pain often radiates from the empty socket to your ear, eye, temple, or neck on the same side of your face where the tooth was extracted. It's a pain that typically isn't relieved by regular pain medication and can be accompanied by a foul odor or an unpleasant taste in your mouth. This distinct timeline and increasing severity are key indicators that distinguish dry socket from the expected discomfort of a healing extraction site.
The Dry Socket Timeline: When Does Pain Actually Start?
Patients frequently ask about the timing of dry socket. While an extraction causes immediate discomfort, the severe pain of a dry socket doesn't appear right away. The typical onset is 3-5 days after surgery, with many cases developing on the third or fourth day. This period is the peak risk for developing the condition.
Why this delay? It's all about the blood clot. After an extraction, a blood clot forms in the socket. It takes some time for this clot to fully stabilize and then, if conditions are unfavorable, to either get dislodged or dissolve. The process of clot dissolution, known as fibrinolysis, can contribute to dry socket, especially if it occurs prematurely. Various factors, which we'll discuss shortly, can accelerate this breakdown or cause physical dislodgement. Therefore, the pain isn't instantaneous but rather a delayed reaction to the absence of this protective clot.
The good news is that the risk of dry socket decreases over time. The longer the wound heals without incident, the lower the likelihood of developing the condition. For most patients, the risk is significantly reduced once the socket begins to close and new tissue forms, typically around 7-10 days post-extraction. This timeline is consistently supported by medical research, with most cases developing within roughly 3-5 days after surgery.
So, Can You Get Dry Socket Same Day as Extraction? The Short Answer
Let's get straight to the point: can you get dry socket same day as extraction? The short answer is, it's highly, highly unlikely, virtually impossible even.
It's understandable to worry about complications when you're in pain after an extraction. However, the physiological process required for a dry socket to develop simply doesn't happen within hours of the extraction.
Dry socket occurs when the protective blood clot is lost, exposing bone and nerves. This clot forms immediately after the tooth is pulled. It then needs time to either be dislodged by external forces (like vigorous rinsing or sucking) or to dissolve prematurely due to internal factors (like infection or certain medications). This process, and the subsequent onset of severe, distinct dry socket pain, requires at least a day, if not more, to manifest.
The pain you feel on the same day as your extraction is normal post-surgical discomfort. It's the body's natural response to trauma, the anesthesia wearing off, and the initial stages of healing. It's important not to confuse this expected soreness with the unique and worsening pain profile of a dry socket.
Why is it rare to get dry socket same day as extraction?
The rarity of developing a dry socket on the same day as extraction is rooted in the very physiology of healing and the nature of the condition itself. Here’s why it almost never happens:
- Immediate Clot Formation: The moment a tooth is extracted, your body's natural defense mechanism kicks in, and a blood clot begins to form in the socket. This clot is usually quite stable in the initial hours, assuming proper post-operative care is followed.
- Time for Dislodgement or Dissolution: For a dry socket to occur, this blood clot must either be physically dislodged (e.g., by excessive sucking, spitting, or smoking) or chemically dissolved (e.g., due to bacterial infection or certain medications interfering with clot stability). These processes take time – typically 24 hours or more – to fully manifest and lead to the exposure of bone and nerves.
- Initial Pain Source: The pain experienced on the day of the extraction is primarily due to the surgical trauma itself. The tissues and bone have been manipulated, and as the local anesthesia wears off, you will naturally feel soreness and discomfort. This is entirely different from the specific, intense pain of a dry socket, which arises from exposed bone and nerves once the protective clot is gone.
- Anesthesia Wearing Off: For several hours after the procedure, the lingering effects of local anesthesia will numb the area, masking any immediate pain that might arise from an exposed socket, even if the clot were to somehow disappear instantly. By the time the anesthesia fully wears off, enough time has usually passed for dry socket symptoms to adhere to their typical 1-3 day onset.
The body needs a bit of time for the critical blood clot to fail before the characteristic symptoms of dry socket can emerge. This is why we emphasize monitoring your symptoms in the days following your extraction, rather than panicking about every discomfort on day one.
Key Risk Factors and How to Prevent Dry Socket
While dry socket is uncommon, certain factors can significantly increase your risk. Understanding these factors is key to prevention.
Here are some key risk factors and essential prevention tips:
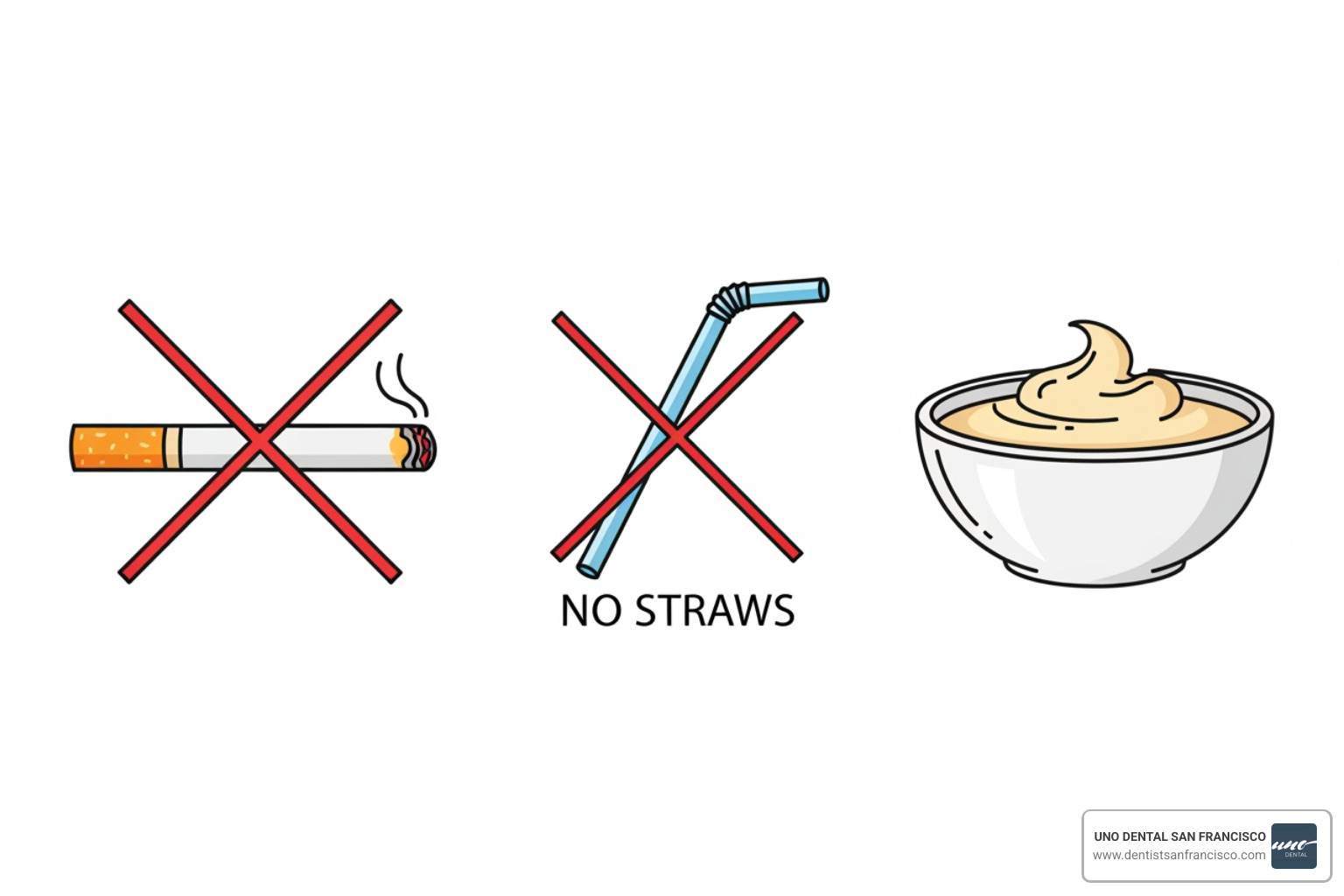
- Smoking and Tobacco Use: This is one of the most significant risk factors. The chemicals in tobacco can interfere with healing and break down the blood clot. Additionally, the sucking motion required to smoke can easily dislodge the clot. A 2022 systematic review highlighted a strong link, showing the incidence of dry socket in smokers was about 13.2% compared to about 3.8% in non-smokers. We advise against smoking or using any tobacco products for as long as possible after your extraction, ideally for at least 48 hours, but longer if possible.
- Sucking Actions (Straws): Using a straw, vigorous spitting, or even sucking on hard candy creates negative pressure in your mouth. This suction can easily pull the protective blood clot out of the socket. Avoid using straws for at least a week after surgery.
- Oral Contraceptives: Oral contraceptives may increase dry socket risk, as estrogen levels can interfere with clot stability. A 2022 systematic review and meta-analysis suggests a significantly higher risk for those using oral contraceptives. If you are on birth control, please inform us so we can discuss specific precautions.
- Difficult or Traumatic Extractions: Extractions that are more complex, such as impacted wisdom teeth or those requiring significant manipulation of the bone, can increase the risk of dry socket. This is because there might be more tissue trauma or a greater chance of clot disruption during the procedure.
- Poor Oral Hygiene: Pre-existing oral infections or generally poor oral hygiene can introduce more bacteria into the extraction site, which can break down the blood clot and lead to dry socket. Maintaining excellent oral hygiene before and after your extraction is crucial.
- Pre-existing Infection: If there was an active infection in the tooth or surrounding gums prior to extraction, the risk of dry socket can be higher.
- History of Dry Socket: If you've had a dry socket before, you're unfortunately more prone to developing it again.
Controllable vs. Uncontrollable Risks
When we talk about dry socket risk factors, it's helpful to categorize them into those you can influence and those you cannot.
Controllable Risks: These are factors where your actions and choices play a significant role in prevention:
- Lifestyle Choices: Avoiding smoking, tobacco products, and excessive alcohol consumption are critical. These habits can directly interfere with healing and clot stability.
- Aftercare Compliance: Diligently following our post-operative instructions, such as avoiding straws, vigorous rinsing, and eating appropriate foods, is paramount.
- Oral Hygiene: Maintaining good oral hygiene, both before and after the extraction, helps reduce the bacterial load in your mouth, which can otherwise compromise the blood clot.
- Diet and Activity: Sticking to a soft food diet and avoiding strenuous physical activity for the recommended period helps protect the healing site.
Uncontrollable Risks: These are factors that are inherent to your situation or the nature of the extraction, which we will account for in your treatment plan:
- Surgical Complexity: Extractions that are more traumatic or involve impacted teeth (especially wisdom teeth, which are more common in the lower jaw) inherently carry a higher risk. We take extra precautions in these cases.
- Patient's Medical History: Certain medical conditions, such as a history of serious illness or cancer, can influence healing capabilities and increase risk. A 2019 analysis of dental records found that dry socket was more common in people with a history of mouth sores, hospitalization from a serious illness, and cancer. It's vital to provide us with a complete medical history.
- Jaw Location: Extractions from the lower jaw, particularly the back teeth, tend to have a higher incidence of dry socket compared to upper jaw extractions.
- Hormonal Factors: As mentioned, oral contraceptives can increase risk due to hormonal influences.
While some risks are beyond your control, understanding them allows us to implement preventive strategies and monitor your healing more closely. For the controllable factors, your commitment to following our guidance is your best defense against dry socket.
Your Post-Extraction Aftercare Checklist
Following our post-operative instructions is the most effective way to prevent dry socket and ensure a smooth recovery. Here is your checklist:
- Gentle Rinsing: Do NOT rinse your mouth on the day of surgery. Starting the morning after, gently rinse your mouth with warm salt water (1/2 teaspoon of salt in a glass of warm water) several times a day, especially after meals, for 3-4 days. Let the water drain out naturally; do not spit forcefully.
- Soft Food Diet: For the first few days, stick to soft foods like yogurt, applesauce, mashed potatoes, and pureed soups. Gradually reintroduce normal foods as comfort allows, but avoid anything hard, crunchy, or chewy that could irritate the extraction site for at least two weeks.
- Avoiding Strenuous Activity: Rest on the day of surgery. Avoid vigorous exercise, heavy lifting, or any activity that increases blood pressure for at least 48 hours, or as advised by us. Increased blood flow can dislodge the clot.
- Proper Gauze Use: If you experience bleeding, bite down firmly on the gauze pads we provide. Change them as needed, usually every 30-45 minutes, until the bleeding subsides. If bleeding continues, a moistened tea bag (the tannic acid helps with clotting) can be used.
- Hydration: Drink plenty of water. Avoid alcoholic, caffeinated, carbonated, or hot beverages for at least 48 hours.
- No Straws or Smoking: As discussed, these are major culprits. Absolutely avoid using straws and refrain from smoking or using any tobacco products for at least 48 hours, ideally longer.
- Pain Management: Take prescribed pain medication as directed. If you're using over-the-counter options, combining acetaminophen and ibuprofen can sometimes be more effective than either alone.
- Oral Hygiene: Brush your teeth gently, avoiding the extraction site for the first 24 hours. After that, carefully brush around the area. Do not probe the socket with your tongue or fingers.
- Ice Packs: Apply an ice pack to the outside of your jaw for 20 minutes on, 10 minutes off, for the first 24-48 hours to help minimize swelling.
By diligently following this checklist, you significantly reduce your risk of dry socket and promote optimal healing. We are always here to answer any questions about your aftercare instructions.
What to Do If You Suspect Dry Socket
Even with diligent aftercare, dry socket can still occur. If you suspect you are developing one, do not panic. It is a treatable condition, and contacting us promptly will bring relief and ensure proper healing.
Here's how to self-assess and when to call us:
- Worsening Pain: If your pain, instead of improving, starts to get significantly worse 1 to 3 days after your extraction, becoming severe and throbbing.
- Visible Bone: If you look into the socket and see exposed bone, or the clot appears to be missing, rather than a dark, intact blood clot.
- Foul Odor or Taste: A distinctly unpleasant taste in your mouth or bad breath emanating from the extraction site can be a sign of dry socket.
- Radiating Pain: Pain that spreads from the socket to your ear, eye, temple, or neck on the same side of your face.
If you experience any of these symptoms, especially the worsening, severe pain, please call UNO DENTAL SAN FRANCISCO immediately. Prompt professional care is key to managing symptoms and ensuring effective treatment.
Immediate Steps for Severe Post-Extraction Pain
While waiting for your appointment with us, there are a few immediate steps you can take to manage severe post-extraction pain, but remember these are temporary measures until you can receive professional care:
- Over-the-Counter Pain Relief: You can continue to take over-the-counter pain relievers such as ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) as directed on the packaging. Sometimes, alternating between the two, or taking them together (if medically advised and safe for you), can provide more effective relief.
- Cold Compress Application: While dry socket pain is nerve-related rather than swelling, a cold compress on the outside of your cheek near the affected area might offer some temporary comfort by numbing the area.
- Avoiding Probing the Socket: Resist the urge to poke or prod the socket with your tongue or fingers. This can introduce more bacteria and further irritate the exposed area.
- Gentle Warm Salt Water Rinses: Continue with gentle warm salt water rinses as advised in your aftercare instructions. This can help keep the area clean and may provide some soothing relief, though it won't resolve the dry socket itself.
These steps are intended to provide temporary relief. The definitive treatment for dry socket requires professional intervention, which we are ready to provide.
Professional Treatment for Dry Socket
When you come to UNO DENTAL SAN FRANCISCO with suspected dry socket, our priority is to alleviate your pain and promote healing. Our professional treatment typically involves a few key steps:
- Socket Irrigation: We will gently flush the empty socket with a medicated mouthwash or saline solution. This cleans out any food debris, bacteria, or other irritants that might be contributing to the pain and hindering healing.
- Medicated Dressing: After cleaning, we will place a special medicated dressing or paste directly into the socket. This dressing usually contains a pain-relieving agent and often an antiseptic. It acts as a protective barrier, covering the exposed bone and nerve endings, and providing immediate pain relief. You will need to return to our office to have this dressing changed periodically, typically every 24-48 hours, until the pain subsides and healing progresses.
- Pain Management Plan: Beyond the medicated dressing, we may prescribe stronger pain medication to help you manage the discomfort, especially in the initial days of treatment.
- Follow-Up Appointments: We will schedule follow-up appointments to monitor your healing, change the dressing, and ensure the socket is progressing toward a healthy recovery.
- Healing Support: We'll reiterate aftercare instructions, emphasizing gentle oral hygiene and a soft diet, to support the natural healing process. In some cases, if there's a concern about infection, we might prescribe antibiotics.
With proper professional treatment, the pain from a dry socket usually improves significantly within a few days, and complete healing can be expected within a week or two. Our team at UNO DENTAL SAN FRANCISCO is committed to providing compassionate and effective care to get you comfortable and back to your routine as quickly as possible.
Your Partner in a Smooth Recovery
While it's reassuring to know you likely can't get a dry socket the same day as an extraction, proper aftercare and professional guidance are key to a comfortable recovery. Understanding the healing process empowers you to take the right steps and know when to seek help.
At UNO DENTAL SAN FRANCISCO, we prioritize patient education, thorough post-extraction instructions, and convenient follow-up options, including free virtual smile consultations when appropriate. Our team uses high-tech diagnostics and a holistic, individualized approach to help you heal quickly and comfortably after tooth removal.
If you have questions about pain after an extraction, think you might be developing dry socket, or are considering having a tooth removed, our dentists are here to help. Request an appointment online to learn more about our comfortable, efficient extractions and comprehensive aftercare.